Marbella Family Medical Blog |
 |
The Marbella Family Medical Blog is a collection of the top questions we've received on our site related to family-medical issues and emergencies in Marbella and the Costa del Sol. We've all been in a situation where a child slips and falls, or develops a questionable rash while playing outside. This blog aims to address those concerns that have become commonplace for families living or vacationing here on the Costa del Sol.
Please note that the Marbella Family Medical content below is only intended to be a guideline and you should immediately consult an expert regarding any medical issues of concern.
If you have a specific question that you'd like to see addressed on the Marbella Family Medical Blog that is not time sensitive, please let us know using our Ask a Question feature located on the bar above. We'll consult with a medical expert and post the result on this Blog.
We'd like to thank the peadiatrics team at Hospital Ceram for their expert responses on the topics below. Enjoy your time in Marbella and always remember - Safety First!
Meningitis | Tooth injury | Jellyfish stings | Bitten by poisonous insect
Have a question or tip about a medical issue in Marbella?
Share your question or tip here - we'll immediately post it so you can get feedback from the community.
What other visitors have said Medical issues
Click below to see contributions from other visitors to this page...
Poisonous Insects in Marbella - Has Your Child Been Bitten? 




- By Dr. Luzdivina Garcia Morales de los Rios
Marbella Family Medical Blog
Marbella Family Medical advice:
The first thing we need to know is that …
Think about your eyes on World Health Day 




Specsavers Opticas on the Costa del Sol are offering free eye tests including a visual health check throughout April for World Health Day.
The stores …
MENINGITIS VACCINATIONS: HOW IMPORTANT ARE THEY? 




The meningococcus or Neisseria meningitides is a gram-negative bacterium cause meningitis and other forms of meningococcal disease such as meningococcemia …
meningitis vaccinations: how important are they?
The meningococcus or Neisseria meningitides is a gram-negative bacterium cause meningitis and other forms of meningococcal disease such as meningococcemia or sepsis.
The bacterium is referred to as a coccus because it is round, and more specifically, diplococcus because of its tendency to form pairs.
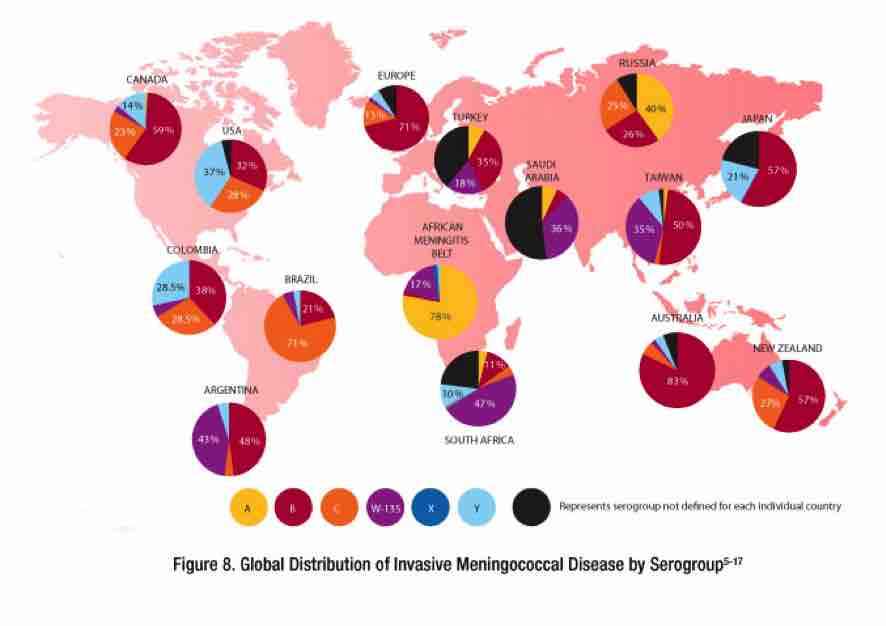
The meningococcus (Neisseria meningitides) is the one with the potential to cause large epidemics. There are 12 serogroups of N. meningitides that have been identified, 6 of which (A, B, C, W, X and Y) can cause epidemics. Geographic distribution and epidemic potential differ according to bacterial serogroups.
incidence & transmission of meningitis
The bacteria are transmitted from person-to-person (is an exclusively human pathogen there is no animal reservoir) through droplets of respiratory or throat secretions from carriers. About 10% of adults are carriers of the bacteria in their nasopharynx. Close and prolonged contact such as kissing, sneezing or coughing on someone, or living in close quarters (dormitory, sharing eating or drinking utensils) with an infected person (a carrier) facilitates the spread of the disease. The average incubation period is 4 days, but can range between 2 and 10 days.
The bacteria can be carried in the throat and sometimes, for reasons not fully understood, can overwhelm the body's defenses allowing infection to spread through the bloodstream to the brain. It is believed that 10% to 20% of the population carries Neisseria meningitides in their throat at any given time. However, the carriage rate may be higher in epidemic situations.
meningitis symptoms
The most common symptoms are a stiff neck, high fever, sensitivity to light, confusion, headaches and vomiting. Even when the disease is diagnosed early and adequate treatment is started, 5% to 10% of patients die, typically within 24 to 48 hours after the onset of symptoms. Bacterial meningitis may result in brain damage, hearing loss or a learning disability in 10% to 20% of survivors. A less common but even more severe (often fatal) form of meningococcal disease is meningococcal septicaemia, which is characterized by a hemorrhagic rash and rapid circulatory collapse.
Diagnosis of meningitis: What you need to know
Initial diagnosis can be made by clinical examination followed by a lumbar puncture showing a purulent spinal fluid and the bacteria can sometimes be seen in microscopic examinations of the spinal fluid.
- The diagnosis is supported or confirmed by:
- Blood or spinal cultures who shows the bacterial growing
- Agglutination tests
- PCR
The identification of the serogroups and susceptibility testing to antibiotics are important to define control measures.
Treatment of meningitis
Suspicion of meningitis is a medical emergency and immediate medical assessment is recommended. Current guidance in the United Kingdom is that if a case of meningococcal meningitis or septicaemia (infection of the blood) is suspected intravenous antibiotics should be given and the ill person admitted to the hospital. This means that laboratory tests may be less likely to confirm the presence of Neisseria meningitides as the antibiotics will dramatically lower the number of bacteria in the body. The UK guidance is based on the idea that the reduced ability to identify the bacteria is outweighed by reduced chance of death.
Appropriate antibiotic treatment must be started as soon as possible, ideally after the lumbar puncture has been carried. If treatment is started prior to the lumbar puncture, it may be difficult to grow the bacteria from the spinal fluid and confirm the diagnosis.
A range of antibiotics can treat the infection, including penicillin, ampicillin, chloramphenicol and ceftriaxone.
prevention of meningitis
The most important form of prevention is a vaccine against N. meningitides. Different countries have different strains of the bacteria and therefore use different vaccines.
Five serogroups, A, B, C, Y and W135 are responsible for virtually all cases of the disease in humans. Vaccines are currently available against all five strains, including the newest vaccine against serogroups B. The first vaccine to prevent meningococcal serogroups B (meningitis B) disease was approved by the European Commission on 22 January 2013. The vaccine is manufactured by Novartis and sold under the trade name Bexsero. Bexsero is for use in all age groups from two months of age and older.
Serotype distribution varies markedly around the world. Among the 13 identified capsular types of N. meningitides, six (A, B, C, W135, X, and Y) account for most disease cases worldwide. Type A has been the most prevalent in Africa and Asia, but is rare/ practically absent in North America. In the United States, serogroups B is the predominant cause of disease and mortality, followed by serogroups C. The multiple subtypes have hindered development of a universal vaccine for meningococcal disease.
meningitis vaccines
Meningococcal vaccines are available in either bivalent (groups A and C), trivalent (groups A, C and W), or tetravalent (groups A, C, Y and W).
- Meningococcal vaccines for group B
- Meningococcal vaccines against group C. Tetravalent A, C, Y and W conjugate
- Meningococcal vaccines for group A
Written by Dr.Luzdivina Garcia Morales
For more information Marbella Family Medical advice on vaccinations, contact Ceram Hospital.
What you need to know when your child damages a tooth

Marbella Family Medical advice:
Teeth injury in children…What to do?
As distressing as it might be for parents, chipped or broken teeth are quite common in kids. These teeth injuries can occur in a wobbly toddler after a hard fall, a sporty preschooler who gets knocked in the mouth by a ball, or a curious youngster who crunches on hard candy. Your child’s injury may be to a baby tooth or a permanent (adult) tooth.
The tooth can be fractured (broken or cracked) or chipped, and sometimes it may not even hurt. If a large piece of tooth breaks off, however, it will probably cause pain, and your child’s tongue may get cut against the sharp, jagged surface. If the break extends into the tooth’s pulp, where the nerves and blood vessels lie, that tooth becomes much more sensitive to hot and cold liquids and food.
Your child’s dentist can recommend the best method of treatment for a chipped or broken tooth. Treatment can depend on the size and location of the break or crack and sometimes, in the case of very small cracks, no treatment is required.
For a chipped baby tooth, your dentist might leave it alone or simply smooth and polish it.
If one of the front teeth gets chipped, the dentist can smooth the jagged edge and insert tooth-colored filling. A permanent tooth may require filling material to stop the damage from getting worse and to help the tooth feel better.
A broken tooth usually involves the whole tooth down to the nerve. Typically, the break can be fixed with a filling to repair the lost tooth structure, but sometimes a crown is required.
What should I do if my child injures a tooth? Marbella Family Medical advice:
- Inspect your child’s mouth to ensure that no pieces of tooth are stuck in the gums, tongue, or lips. Rinse the mouth with water to clean the area.
- If the affected area is bleeding, fold a clean piece of wet gauze on top of the area and tell your child to bite down on it, or simply hold it in place. Apply this pressure for about 10 minutes, or until the bleeding stops.
- Keep a cold cloth on the area to reduce swelling. Your child can also suck on a popsicle to help with the pain and keep the swelling down.
- If possible, collect the chipped pieces and keep them moist in a cup of milk or saliva. In some cases, the dentist can reattach the tooth fragments with special glue.
- Contact your pediatric dentist quickly. If more than half the tooth is broken, the nerve may be exposed and may require immediate attention.
- If necessary, give your child an age-appropriate, over-the-counter pain reliever.
In the case of any tooth injury, contact your dentist right away. If you act fast, you can help to save your child’s tooth and any future potential for extensive dental work.
MarbellaFamilyFun.com would like to thank the peadiatrics team at Hospital Ceram for their expert response on this topic. For more information about dentists in area, check out what the community is saying about recommended dentists in Marbella.
Ouch! What to do about those nasty jellyfish stings

Marbella Family Medical advice:
There is nothing worse than going to the beach with our children expecting a great day, only to hear crying and screaming because something has stung their skin. Weekend over!
Before we get into how to treat a jellyfish sting, it’s first important to understand how jellyfish stings work.
Jellyfish sting you through nematocysts which are released from their tentacles. Nematocysts are tiny spine covered tubules. The spines anchor themselves in your skin and when the nematocysts fire, various chemicals are injected into you. In some cases, you may have thousands of these nematocysts attached to your skin after being in contact with a jellyfish tentacle, not all of which may fire right away. These stingers can continue to release jellyfish venom (poison) into the body.
How should you treat a jellyfish sting?
Most stings can be treated with these simple remedies. If your child is stung:
- Take him or her from the water.
- Rinse the area with seawater. (Fresh water can prompt the stingers to release more venom.)
- Don't rub the area with a towel, as these actions may activate more stingers.
- With some types of jellyfish stings, it helps to soak the area of skin with vinegar for 15-30 minutes.
- Use a credit card to scrape off the stingers still in the skin or apply a paste of baking soda and seawater. Each method may deactivate the stingers of some types of jellyfish.
- If the pain does not disappear, take a pain reliever and an antihistamine.
Call an ambulance immediately if someone has been stung and:
- Is having trouble breathing or swallowing.
- Has a swollen tongue or lips, or a change in voice.
- Has bad pain or feels generally unwell.
- Is nauseated or vomiting.
- Feels dizzy or has a headache.
- Has muscle spasms.
- Has stings over a large part of the body.
- The sting is in the eye or mouth.
Unproved or unhelpfulremedies to avoid:
- Human urine
- Meat tenderizer
- Solvents, such as formalin, ethanol and gasoline
- Pressure bandages
Marbella Family Medical advice on how to avoid a jellyfish sting?
- Reduce your family's chances of a jellyfish encounter by swimming only at guarded beaches, which are more likely to warn visitors about jellyfish.
- Look for a sign or warning flag (some beaches fly a purple or red warning flag when there's "dangerous marine life" in the water).
- You could also consider stashing a small container of vinegar and a plastic card in your beach gear, just in case.
MarbellaFamilyFun.com would like to thank the peadiatrics team at Hospital Ceram for their expert response on Marbella Family Medical topics.
Has your child been bitten by a poisonous insect?

Marbella Family Medical advice:
The first thing we need to know is that any insect who lives in our environment can bite our kids including: mosquitos, spiders, caterpillars, etc.; but not all of them cause a severe reaction.
If your kid has been bitten by a spider or a scorpion, try to identify or take a picture of the insect if this can be done quickly and safely. The insect identification can give us an idea of the evolution and severity.
If you don’t see the insect, or can’t identify it, here are some guidelines to help you know what to do:
- Insect bites and stings can cause immediate skin reaction.
- Bites caused by mosquitoes, fleas, spiders, and mites are more likely to cause itching than pain.
- The bites from fire ants and the sting from bees, wasps, scorpions and hornets are usually painful, localized redness, swelling and also feel burning.
When is it an emergency?
The symptoms vary according to the type of insect and the individual. In most cases, bites and stings can be easily treated at home. However, some children might have a severe allergic reaction to insect bites and stings or some insects can have poison.
We have to suspect the child has a severe reaction (Anaphylaxis) when the symptoms develop quickly, often within seconds or minutes. The following symptoms require immediate urgent emergency care.
Symptoms that require immediate emergency care:
- Abdominal pain
- Abnormal (high-pitched) breathing sounds
- Anxiety
- Chest discomfort or tightness
- Cough
- Diarrhea
- Difficulty breathing
- Difficulty swallowing
- Dizziness
- Light Headedness
- Hives, itchiness
- Nasal congestion
- Nausea or vomiting
- Palpitations
- Skin redness
- Slurred speech
- Swelling of the face, eyes, or tongue
- Unconsciousness
- Wheezing
These severe reactions can be rapidly fatal if untreated. Call immediately for emergency medical assistance: 112 / 061
For emergencies (severe reactions):
- Check the person's airways and breathing. Call 061/112 and begin rescue breathing and CPR (if the victim's breathing or heartbeat has stopped).
- Reassure the person. Try to keep him or her calm.
- Remove rings and constricting items because the affected area may swell.
- Use the person's EpiPen/Jext or other emergency kit, if they have one. (Some people who have serious insect reactions carry it with them.)
- Remain with the person until medical help arrives.
General steps for most bites and stings:
- Remove the stinger if still present by scraping the back of a credit card or other straight-edged object across the stinger. Do not use tweezers, these may squeeze the venom sac and increase the amount of venom released.
- Wash the site thoroughly with soap and water.
- Place ice (wrapped in a washcloth) on the site of the sting for 10 minutes and then off for 10 minutes. Repeat this process.
- If necessary, take an antihistamine, or apply creams that reduce itching.
- Over the next several days, watch for signs of infection (such as increasing redness, swelling, or pain).
Do NOT...
- Do NOT apply a tourniquet.
- Do NOT give the person stimulants, aspirin, or other pain medication, unless prescribed by the doctor.
Prevention
- Avoid provoking insects whenever possible.
- Avoid rapid, jerky movements around insect hives or nests.
- Avoid perfumes and floral-patterned or dark clothing.
- Use appropriate insect repellants and protective clothing.
- Use caution when eating outdoors, especially with sweetened beverages or in areas around garbage cans, which often attract bees.
- For those who have a serious allergy to insect bites or stings, carry an emergency epinephrine kit (which requires a prescription). Friends and family should be taught how to use it if you have a reaction. Wear a medical ID bracelet.
And always remember to ask your doctor!
NOTE: We'd like to thank Dr. Luzdivina Garcia Morales de los Rios, at the Paediatrics Department at Hospital Ceram for the responses provided in the Marbella Family Medical Blog.
Related links to Marbella Family Medical Issues
Below you will find links related to the topics addressed in the Marbella Family Medical Blog:


